Are you interested in becoming a Dental Assistant? Sign up for the best Austin dental assistant school, Star of Texas! What makes Star of Texas Dental Assisting School the best in town? We keep class sizes small so that each student gets a hands-on experience with instructors that truly care so that you are ready to start your career in the dental field.
Students at Star of Texas get to opportunity to learn the ins and out of dental assisting. Let’s take a look at teeth sensitivity.
Teeth can become sensitive for many reasons. Sometimes, the sensitivity is an indication of a potentially serious problem. Other times, the dentally related problem may be small but the effects (the sensitivity) are extremely aggravating.
What do we mean when we say “sensitive teeth?”
Twinges of pain or discomfort in our teeth in certain situations such as drinking or eating cold things, drinking or eating hot things, eating sweets, and touching the teeth with other teeth or the tongue. Your symptoms will involve reactions to temperature or pressure. Sensitivity to cold drinks or foods is the most common symptom.
Two types of sensitivity:
1. Dentinal sensitivity
When the dentin (middle layer) of a tooth is exposed. Normally, dentin is covered by enamel. Dentin becomes exposed when the outer protective layers of enamel wear away. Dentin contains tiny openings called tubules. Inside each tubule lies a nerve branch that comes from the tooth’s pulp (the nerve center of the tooth). When the dentin is exposed, cold or hot temperature or pressure can affect these nerve branches, causing sensitivity.
Causes:
- Inadvertent notching of the tooth surface and/or recession of the gum tissue (exposing the root surface of the tooth) caused by improper brushing: either brushing too hard, brushing with a toothbrush that is too hard, or using an improper brushing technique, which will wear away the enamel layer. This sensitivity can range from mild to extreme; the degree of sensitivity does not appear to be related to the size of the root exposure or notch.
- Poor oral hygiene, allowing tartar to build up at the gum line
- Untreated cavities
- An old filling with a crack or leak
- Receding gums that expose the tooth’s roots, often caused by periodontal disease
- Gum surgery that exposes the tooth’s roots
- Tooth whitening in people who have tooth roots that already are exposed
- Frequently eating acidic foods or drinking acidic liquids
- Purposeful repositioning of the gum tissue during gum surgery can also lead to tooth sensitivity. While recession from brushing is slow, gum recession following gum repositioning occurs very quickly. The portion of the tooth once covered with gum and bone may now be exposed. Root sensitivity in these instances can be quite severe and immediate. It can sometimes last four months or years if not treated.
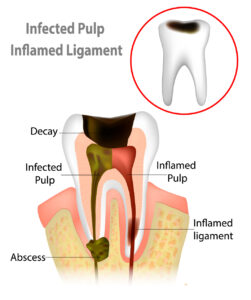
2. Pulpal sensitivity
The reaction of the tooth’s pulp. The pulp is a mass of blood vessels and nerves in the center of each tooth. Pulpal sensitivity affects only a single tooth.
Causes:
- Decay or infection. When a tooth is decayed, temperature changes and sweets will make it sensitive.The solution can be as simple as removing the decay and placing an appropriate restoration.
- A recent filling. A tooth may be sensitive to cold for several weeks after you get a filling. The metals in amalgam (silver) conduct the cold very well, transmitting it to the pulp. Bonded (tooth-colored) fillings require etching the tooth with acid before the filling is placed. In some cases, this etching removes enough enamel to make the tooth sensitive. If a filling is defective or failing, leakage around the filling may cause the tooth to become sensitive.The solution can be as simple as removing the defective filling and placing an appropriate restoration.
- Excessive pressure from clenching or grinding
- A cracked or broken tooth. If the tooth is fractured, you may be sensitive to temperature changes or when chewing food. This fracture condition may be hard to diagnose. If you think you might have this type of sensitivity, read our blog post on “cracked tooth syndrome.”
- A tooth can become sensitive after it has been prepared (drilled) for a restoration (filling). You may have been anesthetized during the procedure, so you did not feel any discomfort when the nerve in the tooth reacted to the heat generated by the drill. The closer the drill comes to the nerve, the more likely it is to cause a sensitivity problem. The high-speed rotation of the bur in the drill generates heat, and the response of the nerve to heat is inflammation. This inflammation is felt by you as a “sensitivity.” If the decay, fracture, or drilling was not too deep, this sensitivity will decrease over time. A week to a month or two is not an unusual length of time for the sensitivity to disappear. A good sign is the continued decrease of sensitivity. However, if the occlusion (bite) is off after the restoration has been placed, the tooth may either become sensitive or may stay sensitive. Once the bite is adjusted, though, the sensitivity should disappear.
- A dying nerve. This can be the result of a deep cavity. Commonly, the sensitive tooth holds an old large filling. The nerve may be damaged during drilling and the nerve has been dying gradually ever since. If this is the problem, the tooth will need endodontic treatment (root canal treatment).
How will the doctor diagnose sensitivity?
Your dentist will look at your dental history and will examine your mouth. You also will need x-rays to show if there is decay or a problem with the nerve. The dentist will ask about your oral habits. Grinding or clenching your teeth can contribute to sensitivity. Your dentist also will look for decay, deep fillings, and exposed root surfaces. During the consultation, your dentist uses an instrument called a spray gun to dispense air across every area of each tooth in order to locate the sensitivity. He or she may use an explorer – a metal instrument with a sharp point – to test teeth
for sensitivity.
How will it be treated?
- Your dentist or dental hygienist will clean your teeth. If your teeth are too sensitive to be cleaned, your dentist may use a local anesthetic or nitrous oxide before the cleaning.
- If there is a notch in the tooth or the shape of the defect is appropriate, the defect is restored (filled in) with a bonded material. This can give immediate relief — sometimes partially, sometimes fully.
- When there is no defect to be restored, the exposed and sensitive root surfaces are covered with a dentin-bonding or other material. This material is invisible and has very little thickness, so you do not notice any change in the appearance of the tooth; but it works. It may have to be reapplied after several months because the bonding material has worn away by tooth-brushing.
- If you have pulpal sensitivity and the tooth’s nerve is damaged or dying, you will need a root canal. Your dentist will remove the nerve and place a non-reactive substance in the space where the nerve was. The tooth will no longer have a continuous barrier of enamel to protect it. Therefore, it will be restored with either a composite filling or a crown.
- Your dentist may apply a fluoride varnish to protect your teeth. This temporarily reduces sensitivity and strengthens your teeth.
- Using fluoride toothpastes and fluoride mouth rinses are home will help to reduce sensitivity. You can also buy toothpastes just for sensitive teeth. You should choose a fluoride mouth rinse that uses neutral sodium fluoride.
How can I prevent it?
- Brush twice a day and floss daily
- Use a soft or ultrasoft toothbrush
- Brush gently up and down, rather than side to side
- Use a fluoride toothpaste and mouth rinse
- Use a toothpaste that protects against sensitivity
- Get treatment for grinding or clenching your teeth (bruxism), like a mouthguard
If you have any questions about tooth sensitivity or have a passion for the dental field and want to sign up to become certified as a Dental Assistant, call Star of Texas Dental Assisting School 512-487-1547